When passed, the Affordable Care Act [ACA] required individuals to purchase & maintain qualifying health insurance coverage – or face a federal penalty. By reducing these penalties to zero in 2019, the federal Tax Cuts & Jobs Act [TCJA] effectively repealed the ACA individual mandate [as distinct from the ACA employer mandate].
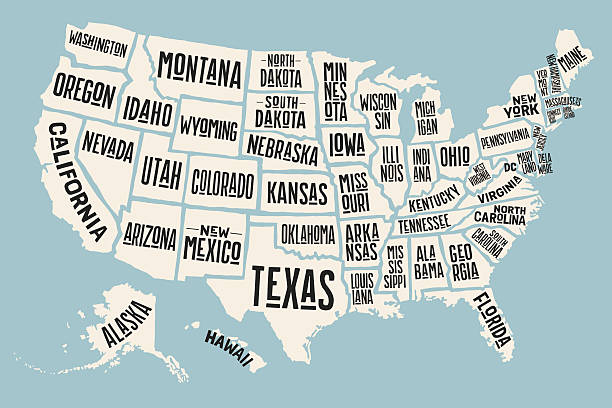
Eleven US states have since formally eliminated the original federal ACA mandate on individuals and implemented [or are in the process of implementing] their own state ACA mandates on individuals in its place.
It is under these eleven state mandates that individual residents are now required to purchase & maintain health insurance – or face state penalties. This arrangement impacts ACA reporting for employers with employees in certain of those states.
Other than in Massachusetts, which has its own reporting system, these states typically gather information about the health coverage by piggybacking on IRS FORMs 1095 & 1094. This means that for certain states, in addition to ACA reporting to the IRS, ALEs must also report health coverage to state governments for any full-time employees resident in those states.
» NOTE: EMPLOYER VS EMPLOYEE LOCATION. The employer organization’s location is not the deciding factor concerning state ACA reporting obligations. The deciding factor is where the employee lives. This adds a layer of complexity for employers with employees who work remotely or commute to work from other states.
Click here for a CHECKLIST of the eleven mandating states, the ACA forms [where specified] to be distributed and filed, and the relevant deadlines.
If you have questions about state ACA mandates & reporting or any other aspect of ACA compliance, please contact BENEFITSCAPE, the leading ACA specialist. BENEFITSCAPE provides best-in-class ACA services & Flag & Fix regtech diagnostics to 1000s of employers across all US states.